Q&A With Ari M. Melnick, MD, on Recent Advances in Lymphoma
Lymphomas are a collection of blood cancers stemming from aberrant lymphocytes, which are critical components of the immune system. Lymphomas are classically divided into two categories – Hodgkin lymphoma (HL), and non-Hodgkin lymphoma (NHL). It is estimated that over 90 percent of lymphomas are NHL, of which there are many distinct subtypes. Recent statistics estimate that nearly 75,000 new cases of NHL will be diagnosed in 2018.
While much still remains unknown about the cause of lymphomas, infection with the human immunodeficiency virus (HIV), the Epstein Barr virus, or the human T-cell lymphotrophic virus can raise the risk of developing lymphoma. Other risk factors include diabetes, obesity, environmental exposure to toxins, and treatment with immunosuppressive drugs following transplants. In addition to family history, gender is an additional risk factor for lymphoma, as men have a higher risk for developing lymphoma than women.
The FDA recently approved the use of CAR T-cell therapy for some patients with NHL, which was covered in detail in this post. Other treatment options for lymphomas include chemotherapy, radiation therapy, and targeted therapy.

Researchers will convene in Boston next week for this inaugural conference centered around malignant lymphoma. Photo: Getty Images
Next week, the AACR is launching a new conference series to discuss the unique challenges and recent advances in the field of lymphoma. The Inaugural AACR International Meeting Advances in Malignant Lymphoma: Maximizing the Basic-Translational Interface for Clinical Application will be held June 22-26 in cooperation with the International Conference on Malignant Lymphoma (ICML). Experts from around the world will gather in Boston to discuss diverse topics, including making inroads into understanding the complexity of the disease and the use of new therapeutic approaches. We had the opportunity to speak with meeting chair Ari M. Melnick, MD, director at the Sackler Center for Biomedical and Physical Sciences at Weill Cornell Medical College in New York about the exciting topics that will be discussed at the meeting.
What’s the broad scope of this inaugural meeting?
We’re trying a hybrid model in this meeting with both official talks and informal dialogue, which I think will create a working-group spirit where people can bring up critiques, ideas, concerns, or proposals and debate them openly. This dialogue will promote interactions and will hopefully advance the field. What really advances science is the opportunity to brainstorm together.
One of the things that I like about this meeting is that it’s incredibly diverse. The research abstracts are on a wide array of topics, ranging from clinical, translational, and basic issues, many with completely new angles that have not been explored before in lymphoma.
What are the biggest challenges in advancing lymphoma research?
There are many challenges. We don’t know much about the mutations that cause lymphoma; the disease has only recently been sequenced, which revealed a heavy mutational burden. Relatively little is known about the mechanistic pathways that, when misregulated, can cause lymphoma.
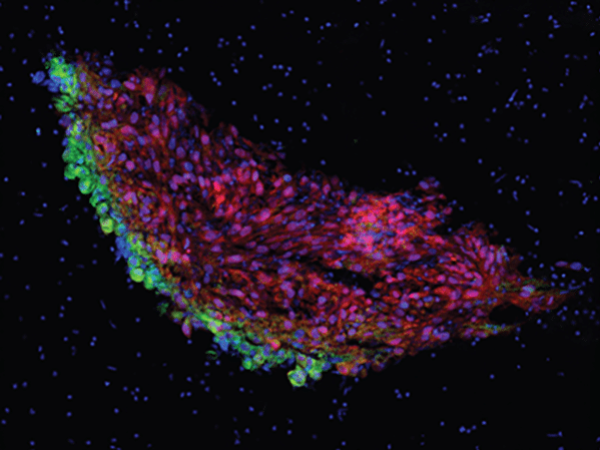
We are starting to understand the immune microenvironment of lymphomas, which is very important, as this is a disease of the immune system. However, we are still trying to understand the full range of immune cell subsets which can become the cells of origin for lymphoma tumors, and how these cells interface with the counterpart immune cells in the host. Some of these issues have recently come to light, and so we will have a lot of discussions in this area.
A subset of lymphomas can be cured with chemo-immunotherapy, which is a tremendous success story for many patients. Nevertheless, we have to move beyond the chemotherapy era and attempt to cure these diseases without using drugs that have long-term toxic side effects and can potentially lead to second tumors. As the accepted standard treatment for lymphoma is chemotherapy, adding new therapeutics is time consuming and expensive. An additional challenge is designing the right preclinical studies to select among the thousands of possibilities of stand-alone and combinatorial therapies that can move in to clinical trials.
Talk about tumor heterogeneity in lymphoma, and how it can affect treatment.
Lymphoma is the king of heterogeneity; that’s been known for a very long time. When I was a resident, lymphoma was known as the ‘great simulator’ because it could clinically appear as any disease, and you had to rule things out to eventually discover that the underlying culprit was lymphoma. Lymphoma is very heterogenous in how it presents clinically and histologically, and pathological classifications have become more and more complicated over the years because of the various histological characteristics. There’s also heterogeneity in terms of the different mutations that can occur in lymphoma; it’s one of the heaviest mutated types of tumors. Furthermore, there is heterogeneity among the cells within each patient’s tumor.
All of this heterogeneity leads to tremendous complexity, and we are working on understanding how this heterogeneity alters our therapeutic approaches.
How do you see immunotherapy fitting into the treatment armamentarium for lymphomas?
I think that immunotherapy is going to be a cornerstone for treatment of lymphoma, but immunotherapy in the context of lymphomas is different than immunotherapy in other cancers.
Solid tumors, for example, arise from tissues that are not part of the immune system, therefore we can use immunotherapy to stimulate the immune system to attack the tumor. Lymphomas, on the other hand, are part of the immune system themselves, so immunotherapy in this context is conceptually interesting and different. For example, small molecules that block the activity of certain mutations in lymphomas that modulate B-cell or T-cell interactions with the rest of the immune system is really a type of immunotherapy. We know that many mutations disrupt the ability of aberrant immune cells to interact with normal host immune cells. Restoring that activity would be considered an immunotherapeutic approach as well.
What are some of the strategies for targeting the aberrant epigenome in lymphoma patients?
This is one of the major growth areas in recent years in the treatment for lymphomas. The first epigenetic targeted therapy for lymphoma is a drug that targets EZH2, a protein involved in histone modification. Many lymphoma patients have EZH2 mutations in their tumors, and this is the first treatment to target this aberrant mechanism. But there are many other epigenetic targets in lymphoma. Recent approaches include targeting specific regulators of the epigenome, as opposed to broadly targeting multiple molecules with older generation drugs such as histone deacetylase (HDAC) inhibitors.
What are some recent treatment breakthroughs?
Some of the exciting treatments that are coming to fruition include CAR T-cell therapy, bispecific antibodies, and the continued improvement of drugs that target signal transduction pathways that lymphomas rely on. Further, some agents being tested in clinical trials for other cancers could be beneficial to many lymphoma patients because they target certain somatic mutations that are also present in lymphoma. With the introduction of some of these new agents, we’re at the point where we can really start thinking about doing basket or matched trials for lymphoma.
Interested in reading more about the latest research on lymphoma? Check out this collection of impactful articles handpicked by the AACR journal editors.
Melnick further shared his expectations for the conference in a video interview.
https://www.youtube.com/watch?v=TKHxV7cQe1Q